
 |
|
What are they, and when do you use them?
by Lawrence Martin, MD
CPAP and BiPAP are used to treat patients with a variety of medical conditions 'non-invasively', i.e., without endotracheal intubation. These conditions include some cases of respiratory failure and pulmonary edema, COPD exacerbation, and most patients with clinically significant sleep apnea. Everyone who routinely cares for acutely ill patients is at least passingly familiar with CPAP and BiPAP. The same is true for those who manage patients with sleep apnea, including sleep lab technicians and sleep physicians.
Over the years I have found that, while many care givers are 'familiar' with CPAP and BiPAP -- including those who prescribe the modalities -- they are often unsure about several issues, including:
My web site is designed to answer these and other questions about CPAP, BiPAP and ASV. The information should be useful to anyone -- student, nurse, sleep lab technician, physician -- who wants to review this complex subject or learn it from scratch. I use the tabular format for comparisons since it's the most instructive (better than paragraphs of prose). Under each modality are multiple links to further information.
Sea Level Air Pressures
760 mm Hg
1033.6 cm H2O
101.1 kPa
14.7 lbs./square inch
The familiar "760 mm Hg" means that the weight of the air at sea level will support a column of mercury 760 mm in height, as shown below. In this figure blue is mercury, and the distance from 'B' to 'A' is the barometric or air pressure. If the open pan of mercury is at sea level than the height of the column (from 'A' to 'B') is 760 mm Hg and the sea level air pressure is said to be '760 mm Hg'.
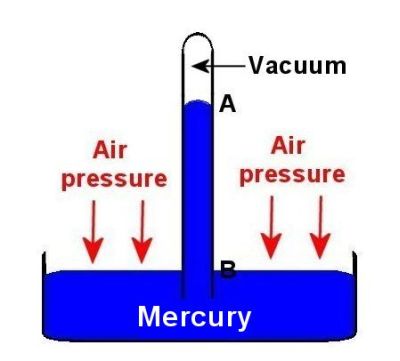
If the blue represented water, then the column would be 1033.6 cm from A to B. and the air pressure would be '1033.6 cm H2O'. In some countries kPa (kilopascals) is used to express pressure, so sea level pressure would be 101.1 kPa.
Yet another way to express air pressure is the weight of all the air over a single square inch of earth's surface. This column, about 70 miles high (the entire earth's atmosphere), weighs at sea level 14.7 lbs., so air pressure at sea level is '14.7 lbs./sq. inch'.
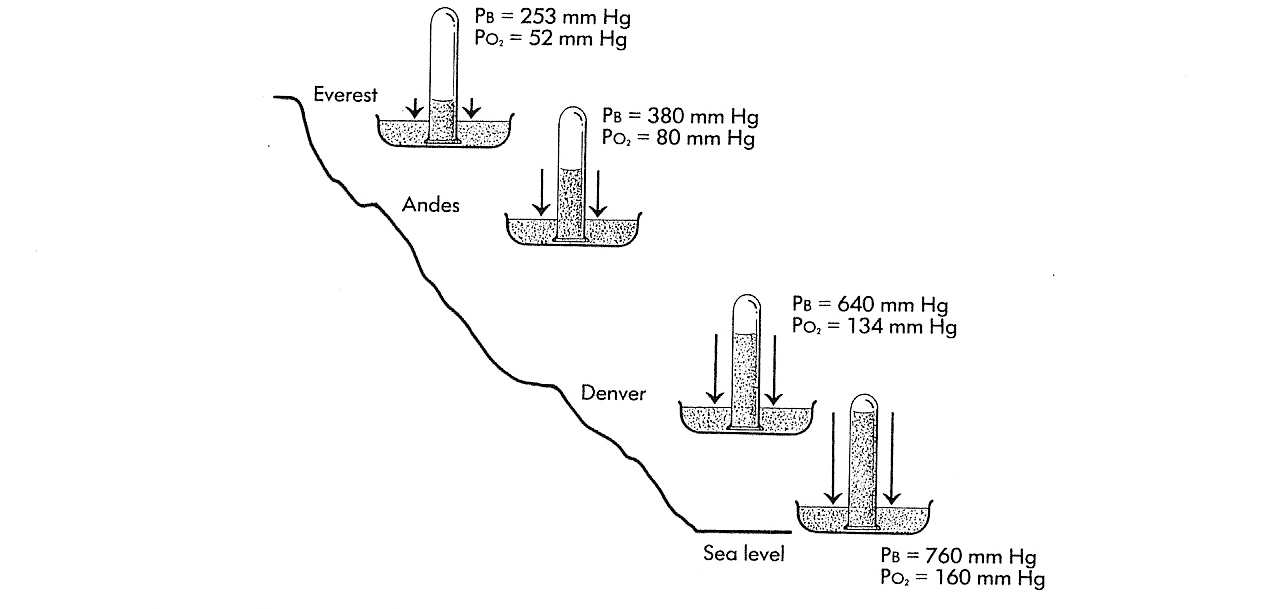
The ambient air pressure decreases with altitude, simply because as you go higher, there is less quantity of air to weigh on the surface. This is shown in the next figure, where PB is the barometric pressure at a given altitude. (PO2 is the partial pressure of oxygen at that altitude, which is not germane to this discussion. Figure is from Chapter 2, Martin L. Pulmonary Physiology in Clinical Practice, Mosby, 1986.)
We breathe by contracting respiratory muscles (mainly the diaphragms) to expand the thorax and thereby create a slightly negative airway pressure relative to ambient pressure. This slightly negative pressure -- about -3 cm H2O at rest -- allows fresh air to enter our lungs and supply the blood with oxygen. Then we relax the respiratory muscles, and in so doing exhale to create a slightly positive pressure relative to ambient (+3 cm H2O); this allows stale air full of carbon dioxide to leave our lungs and enter the atmosphere.
To simplify the numbers for these pressure changes we always reference
ambient pressure to zero. This has two great advantages:
1) We don't have to use large numbers to show the change in airway pressures during breathing;
2) Though the ambient pressure changes with altitude (lower the higher
up you go), zero as the reference point can be used at any pressure.
In other words, since the ambient pressure is distributed evenly thoughout out lungs,
zero can be the reference point for any altitude. Below is a normal pressure
curve during quiet breathing -- likely the way you are breathing, right now.
On inspiration you contract and lower your diaphragms, creating a
transient negative pressure (-3 cm H2O) in the airways; this negative pressure allows
air to flow into the lungs. At the end of inspiration the air pressure has equilibrated with
ambient or '0'; at that point you you relax the diaphragms,
pressure rises slightly above ambient (+3 cm H2O) and you exhale stale air.
Without referencing these pressues to 'zero' for the ambient pressure, we would have to use much higher numbers, and the numbers would change depending on the altitude (and to a lesser extent on weather-related variations in barometric pressure at a given altitude). At sea level ambient pressure is 1033.6 cm H2O, so peak inspiration would be 1033.6-3 = 1030.6 cm H2O, and peak expiration 1033.6 + 3 = 1036.6 cm H2O. In Denver we'd have to use 640 cm H2O, so inspiration would be 637 cm H2O and expiration 643 cm H2O, etc. Obviously it is best to just reference changes in airway pressure to zero and not deal with such big numbers.
With this bit about ambient pressure out of the way, we can now discuss the differences between CPAP, BiPAP and ASV.
CPAP vs. BiPAP vs. ASV |
TOPIC |
CPAP |
BiPAP |
ASV |
Definition |
CPAP is continuous positive airway pressure. It is used via a tight fitting facial appliance ("face mask") to treat obstructive sleep apnea, plus some acute medical problems in hospitalized patients (see Principal Indications, below). With CPAP the patient is exposed to an airway pressure above the ambient or room air pressure, which is always referenced to zero. Thus a CPAP of 5 cm H2O means the patient is continually breathing against an airway pressure 5 cm H2O above the ambient or 'zero' pressure. The pressure curve (see below) looks the same as if breathing at ambient pressure, so that inspiratory and expiratory pressure are still below and above the baseline, respectively. Because the pressue is set at some specific level above ambient (usually in the range of 5 to 15 cm H2O) CPAP can be thought of as 'uni-level' positive airway pressure (though it is never called that), to distinguish it from bilevel positive airway pressure or BiPAP. |
BiPAP is bilevel positive airway pressure. It is also used to treat sleep apnea patients, as well as some acute medical problems in hospitalized patients (see Principal Indications, below). The same types of facial appliance ("face mask") used for CPAP are also used for BiPAP. Whereas CPAP sets a single pressure above the ambient pressure, BiPAP sets two pressures above the ambient, a higher (IPAP) and a lower (EPAP), e.g., 10/5 cm H2O (see pressure curve, below). In BiPAP the higher pressure is experienced on inspiration and the lower pressure on expiration. Note that both pressures are always above ambient. |
NOTE: This table compares CPAP, BiPAP and ASV. For a more detailed discussion of ASV, including comparison of the devices manufactured by ResMed and Respironics, Click here.
ASV stands for adaptive servo ventilation. The devices that deliver ASV
are currently available from only two companies:
ResMed Corporation and
Philips Respironics.
ASV is for patients with sleep apnea conditions that don't respond
to CPAP or BiPAP. Rather than making the patient breathe against a fixed pressure,
ASV actually monitors how much
air the patient is exhaling, and adjusts the next breath accordingly,
to give enough pressure to treat the sleep apnea.
Adaptive Servo Ventilation (ASV):
|
Pressure Curve Examples |
|
|
|
History |
|
BiPAP was developed in mid 1990's by Respironics Corporation, trademarked 'BiPAP'. Since BiPAP is a trademark, other companies use different terms, such as 'bilevel', VPAP (variable positive airway pressure), and "duo." One internet ad shows 4 different bilevel machines from 4 different manufacturers; only Respironics' machine is "BiPAP." |
At some point in the late 1990s ResMed Corporation developed an ASV machine, and had it tested in heart failure patients with Cheyne-Stokes respiration. C-S respiration, a waxing and waning resipratory rate with periods of apnea, often occurs during sleep in patients with congestive heart failure. The first clinical article to appear on ASV was Teschler H, et al. Adaptive pressure support servo-ventilation: a novel treatment for Cheyne-Stokes respiration in heart failure. Am J Respir Crit Care Med 2001;164:614-9. Over the next decade more articles appeared showing that ASV
could treat not only Cheyne-Stokes respiration, but a syndrome that wasn't even
recognized in 2001: Complex Sleep Apnea, which is the intrusion of central sleep apneas
when some patients are treated for OSA with CPAP or BiPAP. For later reviews
see:
|
Principal Indications
|
Non-acute setting: Treatment of obstructive sleep apnea. Acute setting: Pulmonary edema or COPD exacerbation, when there is hypoxemia but not CO2 retention. Note: CPAP by face mask = PEEP in the intubated patient. |
Non-acute setting:
Acute setting: Pulmonary edema or COPD exacerbation, when there is CO2 retention and a desire to avoid endotracheal intubation. Note: BiPAP by face mask = PSV + PEEP in the intubated patient. |
Non-acute setting: 1) Central sleep apnea unresponsive to CPAP or BiPAP. 2) Complex sleep apnea. Acute setting: Very rarely (see ACUTE SETTING, below). |
How is the pressure applied non-invasively? |
Via a tight fitting mask attached in such a way that air can be blown into the nose or the nose and mouth (see mask photos below). The mask connects to a hose that is attached to a CPAP machine |
Same as with CPAP, but machine used is designed to deliver BiPAP. |
Same as with CPAP but machine used is designed to deliver ASV. |
What kind of mask is used? |
The mask choices are the same whether the patient is using CPAP or BiPAP. Generally there are 3 types: nasal mask, nasal pillows, and full face mask. (See special situation for mask under ASV.)(The nasal mask (left) and nasal pillows (right) can be used with CPAP or BiPAP.)
|
Same as for CPAP(The full face mask shown can be used with CPAP, BiPAP or ASV.)
|
Same as for CPAP. However, ResMed specifies their brand of full face mask for the ResMed VPAP AdaptSV machine. See Typical Prescription, below. |
Typical Prescription
|
CPAP at 10 cm H2O via best-fit mask [nasal or other], with heated humidity |
BiPAP at 12/8 cm H2O via best-fit mask [nasal or other], with heated humidity.In this prescription the higher number is IPAP (inspiratory positive airway pressure) and the lower number is EPAP (expiratory positive airway pressure)
|
ResMed VPAP Adapt SV: EPAP [expiratory positive airway pressure]
= 7.0 cm H2O, Minimum PS [pressure support] =
4.0 cm H2O, Maximum PS = 13.0 cm H2O, via ResMed Quattro Full Face Mask
(mask recommended by ResMed with this machine), with heated humidity. Below is the ResMed
ASV machine.
|
Medicare Coverage Guidelines(To some extent these guidelines also influence almost all commercial insurance coverage) |
|
|
The following information is from the CMS web site on Respiratory Assist Devices
for Central sleep apnea, defined as:
for Complex sleep apnea
[NOTE: CMS defines an hypopnea as "an abnormal respiratory event lasting at least 10 seconds associated with at least a 30% reduction in thoracoabdominal movement or airflow as compared to baseline, and with at least a 4% decrease in oxygen saturaiton." This definition makes the CMS criteria for central sleep apnea and CompSA confusing, because hypopneas are not traditionally scored as obstructive or central, but simply 'hypopneas'. Thus by CMS criteria a patient could have persistently high AHI from obstructive hypopneas after a CPAP/BiPAP titration, yet qualify for an ASV machine. One doubts that was the intent of the stated criteria.] |
Confusing Points Clarified |
CPAP is often discussed under the general subject of non-invasive ventilation but CPAP does not, technically, provide 'ventilation' to the patient. It sets a single higher ambient pressure against which the patient breathes, but does not (or is not designed to) augment alveolar ventilation. Thus if your goal is to improve someone's PaCO2 non-invasively (i.e, to treat hypercapnia), CPAP is not the method of choice; instead, BiPAP is recommended.Another clarification about CPAP is that it is a generic term, not any manufacturer's trademark, like BiPAP and ASV. It is offered on machines from multiple companies, all of whom may use the term 'CPAP'. (See 'Typical Prescription', above.) Manufacturers may embellish their CPAP with little twists which are patented, and seldom adequately explained. An example is Respironics' CFlex and CFlex+. They are 'pressure relief' modes that abruptly drop the pressure in the transition from inspiration to expiration, to a sharper degree than would occur with passive exhalation. The mode is designed to make CPAP more comfortable for the patient and improve overall compliance (Nilius et al, 2006 and Dolan et al, 2009). CFlex comes in 3 levels, 1, 2 and 3, representing roughly 1, 2 or 3 cm H2O drop in pressure. CFlex+ is supposed to be an advance over regular CFlex. Finally, 'CPAP' is mis-used for a ventilator mode on the Puritan-Bennett
7200 ventilator, as shown in the bottom row of the PB-7200 panel (3rd from left).
The 'CPAP' mode on the 7200 is for the spontaneously breathing patient, who may or may not be receiving CPAP. Thus the CPAP mode on the 7200 can allow for CPAP, PSV (pressure support ventilation), PSV with PEEP (same as BiPAP) or simply normal breathing with no increase in airway pressures (though the patient is still intubated). |
BiPAP is used for non-invasive ventilation. It is designed to augment alveolar ventilation because it delivers two pressures, one higher (IPAP or inspiratory positive airway pressure) and one lower (EPAP, or expiratory positive airway pressure); however, both IPAP and EPAP are above ambient presure. BiPAP is the same as PSV + PEEP in the intubated patient.BiPAP is actually a trademark of Philips Respironics, and so cannot be used in advertising by other manufacturers. ResMed Corporation, for example, uses the term "Bilevel" instead of BiPAP. Many machines are on the market that can deliver BiPAP (see 'Typical Prescription' above). Also confusing is that BiPAP comes in several 'modes' -- all variations on the simple two pressure model:
Respironics also has a BiPAP machine designed specifically for patients with hypoventilation disorders (e.g., restrictive thoracic disorders, obesity hypoventilation syndrome, some cases of central apnea and COPD). It is called BiPAP AVAPS. AVAPS stands for "Average Volume Assured Pressure Support," and is basically a mode for giving non-invasive ventilation to patients with hypoventilation. Not to be confused with ASV (see next column), AVAPS is not for complex sleep apnea or sleep apnea unresponsive to CPAP and BiPAP (which are the indications for ASV). This type of device, while theoretically important in a niche market, does in fact overlap with regular BiPAP and ASV, and so can confuse the overall picture of positive pressure devices (see Recommendation, below). While BiPAP is generally better than CPAP for patients with CO2 retention, or who need augmentation in alveolar ventilation, there is no rule of thumb about which BiPAP mode is 'best'. That can only be determined with a careful titration of pressures in the hospital or sleep lab. |
ASV is a CONFUSING term, for several reasons.1) It is a manufacturers' proprietary trademark, owned by ResMed Corporation. ResMed was the first company to come out with this type of 'smart' machine, which is designed (and Medicare-approved) for treatment of central sleep apnea and complex sleep apnea. 2) Another equipment company, Philips Respironics, has come out with a competing machine for the same set of conditions. Respironics calls its machine BiPAP-autoSV, which stands for 'automatic servo ventilation.' Obviously this is also 'ASV' but Respironics can't market their machine as 'ASV' and they always use the term "autoSV". 3) The algorithms that govern these machines are both proprietary, which means they can't be duplicated by any other machines on the market. 4) The manufacturers use a variety of abbreviations, often without explanation, in their brochures and web sites. Sometimes they use "EEP" (end-expiratory pressure) to indicate what is more commonly called "EPAP" (expiratory positive airway pressure), and "PS" (pressure support) to indicate "IPAP" (inspiratory positive airway pressure). At other times they will use EPAP, IPAPmin, IPAPmax. EPAPmin and EPAPmax. When you add this variety of pressure abbreviations to 'ASV', 'autoSV', VPAP, etc., the result is often a mishmash of confusing lingo. I have yet to see a brochure or web site that lists all the abbreviations alongside equivalent terms and full text explanations. (The companies have great engineers but need better writers.) 5) Though ASV is a proprietary term, being first on the market, it is now used generically to mean 'a machine that is designed to treat central or complex sleep apnea'. Thus if you send a patient to the sleep lab for 'titration with ASV', and the lab has only the Respironics autoSV, that machine will likely be used for the pressure titration. You will get a report of ASV titration with Auto-SV. (An analogy is "Band-Aid", which is a trademarked term by Johnson & Johnson but used by everyone to mean a small tape bandage sold in stores.) In summary, ASV-type machines are an evolving technology, and the terminology is not as well defined as it is with BiPAP and CPAP.
Unless specifically stated otherwise, ASV in this web site can be inferred to mean ResMed's or Respironics' ASV devices. Click here for a table comparing the two companies' ASV devices.
|
What are the principal uses in the ACUTE SETTING? |
In the ACUTE SETTING, CPAP is used for patients with low oxygen saturation in whom O2 at ambient pressure (nasal cannula, loose fitting face mask) is not sufficient. The increased ambient pressure provided by CPAP 'recruits' or opens up more alveoli, allowing supplemental oxygen to better oxygenate the blood. Conditions commonly treated with CPAP in the ACUTE SETTING include pulmonary edema (cardiac and non-cardiac) and COPD exacerbation. If the condition doesn't improve and CPAP is not effective, generally the next step is intubation and mechanical ventilation.There are three broad criteria for CPAP in the ACUTE SETTING:
1) The patient must have a dangerously low SaO2 that cannot be corrected with
supplemental oxygen delivered high-flow, loose-fitting mask.
|
In the ACUTE SETTING, BiPAP is used for patients with high PaCO2 (hypercapnea) when it is causing either respiratory acidosis and/or hypoxemia, and the sitaution is expected to stabilize with medical therapy. The most common condition treated with BiPAP in the ACUTE SETTING is COPD exacerbation. However, any other condition that may lead to hypercapnea can also be treated with BiPAP. Generally, if the condition doesn't improve and BiPAP is not effective, the next step is intubation and mechanical ventilation.As with CPAP, there are 3 broad criteria for BiPAP in the ACUTE SETTING:
1) the patient mush have dangerously high PaCO2
that the physician feels should be lowered as quickly as possible, without endotracheal intubation;
|
ASV via face mask is not used in the acute setting. ASV as a ventilatory mode in intubated patients is used occasionally. One study (Intensive Care Med. 2010 Aug;36(8):1371-9. Epub 2010 May 26. Adaptive support ventilation versus conventional ventilation for total ventilatory support in acute respiratory failure. Iotti GA, et. al.) found that "Comparison between ASV and CV [controlled ventilation] resulted either in similarities or in minor differences. Except for excessive Vt in a few obstructed patients, all differences were in favor of ASV." |
What are the principal uses in the NON-ACUTE SETTING? |
In the NON-ACUTE SETTING, CPAP is used almost exclusively for obstructive sleep apnea (OSA). There are degrees of severity for OSA, but generally the more severe the condition, the more likely CPAP will be prescribed and the more efficacious it will be for the patient. Note that CPAP is generally not helpful in patients with central sleep apnea (CSA). For CSA, BiPAP or ASV are indicated. |
In the NON-ACUTE SETTING, BiPAP has 3 main uses: 1) For obstructive sleep apnea (OSA) that does not respond to CPAP. Either there is patient intolerance to the fixed pressure, or the patient just needs two levels of pressure to eliminate the apneas. In these situations BiPAP is often effective. 2) BiPAP is generally more effective than CPAP in central sleep apnea (e.g., Cheyne-Stokes breathing). 3) BiPAP is sometimes used for patients with chronic hypercapnia, for augmentation of oxygenation and ventilation during sleep. Examples include patients with neuromuscular impairment (post-polio syndrome; amyotrophic lateral sclerosis). Click here for brief introductory youtube.com video about BiPAP |
ASV is currently used almost exclusively in the NON-ACUTE SETTING setting, for patients with 'complex sleep apnea'. CompSA, as it's abbreviated, is defined as central sleep apnea that appears when obstructive sleep apnea is treated with CPAP or BiPAP. Thus, ASV is indicated for situations when CPAP or BiPAP has failed. Even so, it remains somewhat unsettled about when ASV should be used, how effective it is, and how to follow up such patients. |
What is the cost in the non-acute setting? |
It depends on who is paying. There is no meaningful way to make cost comparisons, because patients rarely pay out of pocket for these machines. The cost is paid by either Medicare, Medicaid or commercial insurance companies. There are many web sites for purchasing these machines, such as cpap.com, CPAP-Supply and The CPAP Shop.At cpap.com you will find prices ranging from @$200 for a basic CPAP machine to $5800 for 'smart' or ASV-type machines (not counting mask, which is extra). In clinical practice patients usually get their machine from a a DME (durable medical equipment) company, whose cost is higher than on the internet because they provide service to the machines and training to the patient. Even so, DME companies will generally accept whatever the insurer pays, as long as it covers their cost. The insurer will sometimes rent the machine from the DME company, sometimes buy it outright, and there may or may not be a deductible to the patient. Thus there is no simple answer. Note that the equipment costs DO NOT include the cost of the sleep study needed to make the diagnosis, or the physician's professional fees. In a typical scenario (one or two nights in a sleep lab, professional fees, all equipment) the total cost to diagnose and treat sleep apnea with a basic CPAP device is likely around $4000 - $5000. Since this is a non-recurring charge, and can in the long run prevent many costly and serious medical problems for the patient, insurers routinely cover most or all of the costs. |
See comments under CPAP. |
Same comments under CPAP. |
Recommendation: ONE machine for all |
In the last decade there has been explosive growth in the field of sleep medicine and positive
pressure devices used to treat patients with OSA, CSA and ComplexSA. Machines have become
smaller and quieter, which is a good thing. They have to some extent also
become commoditized, and are available for sale on numerous web sites, including ebay. At the same
time the manufacturers have introduced a plethora of 'machine types' which keep prices for the newer
machines high and serve to confuse the consumer. In this case the consumer is both the patient AND
the physician who must write the prescription. Consider this current line up of positive pressure devices
for patients with sleep disorders from just one company,
Respironics.
These 6 different machines all work the same, delivering postive pressure from a small box. The differences reside in the algorithms used to deliver the pressures. They could all be in one machine. This is the situation with a hospital ventilator, as used in the ICU: one machine that delivers any mode of ventilation the patient needs. Doctors don't keep changing the ventilator machine when the mode changes. ALL of the modes are built into one machine. Is this feasible for the small machines used to treat patients with sleep apnea? Not only is it feasible, it exists! It's the lab version of the machines, the one used in the sleep lab to 'titrate' pressures to the level needed, depending on the situation It's called the OmniLab, a machine that has most of the modes built in. Respironics states "many therapy modes and Respironics' patented comfort technologies are available for titration of almost any patient type, including pediatric patients ages seven and older, in CPAP; BiPAP S, BiPAP S/T, T and PC modes." But the Omnilab is not sold for home use. There is no consumer version of the Omnilab. We need ONE machine for patients with sleep disorders, with all modes built in. Not 6 different machines and over a dozen different models from just one company. The only valid objection is that the high tech machines cost more, and that the companies can't sell one machine at one price with a wide range of functions and still make a profit. This objection is easily overcome by charging for the program used, not the machine. Just as several people with the same identical cell phone can pay different rates depending on the service (phone calls only, internet access + phone, etc.) the charge could be based on the modality used: more for ASV and less for simple CPAP. The sleep community needs an all purpose positive pressure machine that can do everything, whatever the clinical circumstance, and not this plethora of confusing, overlapping machines that are all too often poorly understood. Such an approach from industry might even sell more machines, especially if prices come down, and patients realize they can try different modalities while at home, without obsoleting their existing machine. |
See comments under CPAP. |
Same comments under CPAP. |
ABBREVIATIONS (alphabetical order)
|
Return to table: CPAP vs. BiPAP vs. ASV
Return to Lakeside Press home page
Forward any comments to:
larry.martin@roadrunner.com